Discover advanced therapies, tailored to your needs, that can be delivered in our clinics, at home, or onsite at your workplace.
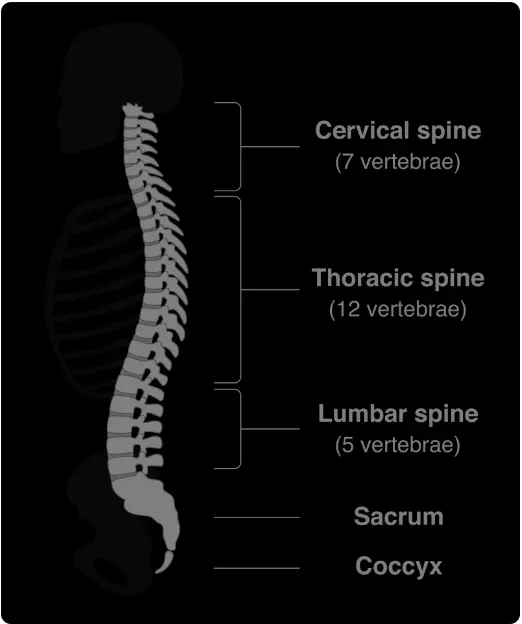
Back and spine pain encompasses a wide range of conditions, from acute injuries to chronic pain. It can affect any of the five major sections of the back: cervical, thoracic, lumbar, sacral, and coccyx.Back pain is the most common reason for surgeries, the leading cause of disability, and one of the most significant medical expenses in the U.S. Addressing the root causes is essential to achieve long-term relief and avoid unnecessary procedures.

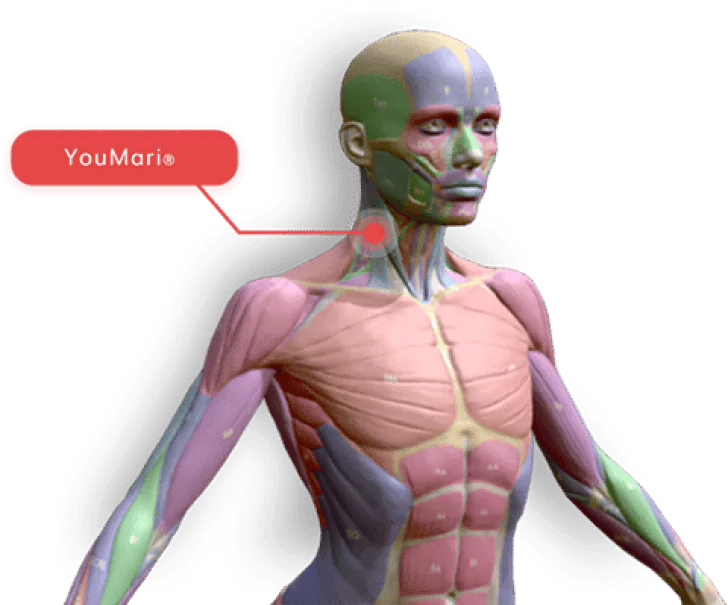
The cervical spine is the uppermost section of the spine, consisting of seven vertebrae (C1-C7) located in the neck region. It provides support to the head and allows for a wide range of motion.
The thoracic spine is the middle section of the spine, comprising twelve vertebrae (T1-T12) located in the upper and middle back. The thoracic spine connects to the rib cage and provides stability to the upper body.
The lumbar spine is the lower back region, consisting of five vertebrae (L1-L5) that hold the majority of the body’s weight. The lumbar spine provides flexibility and supports movements such as bending, twisting, and lifting.
The sacrum is a triangular bone located below the lumbar spine, composed of fused vertebrae (usually five) that connect the spine to the pelvis. It forms part of the pelvic girdle and provides stability and support.
The coccyx, commonly known as the tailbone, is a small, triangular bone located at the base of the spine. It consists of three to five fused vertebrae and serves as an attachment point for various muscles and ligaments.
Back pain can have various causes and most commonly experienced in the lower back region (lumbar spine), including:
Poor posture: Prolonged periods of sitting or standing with improper posture can strain the back muscles and cause discomfort.
Injury or trauma: Accidents, falls, or sports injuries can damage the structures in the back and cause pain.
Herniated or bulging discs: The discs between the vertebrae can rupture or bulge, pressing against nearby nerves and causing pain.
Our treatments harness the power of science-backed regenerative medicine to stimulate your body’s natural healing processes. Delivered in clinics, at home, or onsite, our therapies include:

Our Regenerative Therapies our Not the Alternative, they are the
BEST CHOICE
Experience hands-on care and advanced regenerative therapies in a relaxing, state-of-the-art environment.
Continue your healing journey with easy-to-use devices designed for at-home therapy.
Bring regenerative medicine to your workplace, improving employee health and productivity.
We are committed to personalizing treatment plans based on what is best for every individual’s UNIQUE circumstances to include symptoms, budget, lifestyle, and goals. Conservative (non-surgical) care is effective in resolving pain and injuries most of the time.
We will evaluate your health history, symptoms, and conduct functional movement tests to help determine the severity of your condition. We may use our patented 3D mobility health assessment tool to objectively measure and baseline your range of motion and stability of joints.
If your condition qualifies for conservative care options, we will present a treatment plan that includes only those modalities proven to be effective in treating your condition. This may include shockwave, PRP, light therapy, and fascial manipulation. You will be provided with at least treatment plan options and timelines with transparent out of pocket costs to you.

More than 62% of chronic and over 78% of acute back pain is resolved with conservative care delivered over a period of time mutually agreed to fit your schedule. Conservative care treatments work best when spread out over a 3 to 6-week period to allow adequate healing between treatment modalities
If your symptoms and condition is not eligible for conservative care, or conservative care did not produce the desired outcomes, we start with an expert/accurate diagnosis from our medical doctor pain specialists. Our medical director (6-time patented medical device inventor) will personally conduct a 90-minute comprehensive evaluation to include reviewing available imaging resulting in an accurate diagnosis and personalized treatment plan options.

Our goal is to resolve pain, improve strength, and improve range of motion without surgery. We are consistently successful in achieving this in over 90% of cases. In those rare cases in which surgery is necessary we will guide you by finding the right surgeon we trust for your particular injury and circumstances. We are your independent experts and not financially motivated to conduct surgeries.
Shockwaves can accelerate the healing process in the body, they stimulate metabolism and improve blood circulation; allowing damaged tissue to regenerate and fully heal. When properly applied, shockwave therapy can take a chronic condition back into the acute phase of healing. Chronic pain is caused by an incomplete healing process which must be disrupted (signaled) to be resolved (fully healed). ESWT has been used and studied in clinical applications since 1980, first emerging as a noninvasive procedure to breakup kidney stones. Treatment is noninvasive and virtually painless. The provider moves a handpiece around the pain zone and through the wand, low-energy shockwaves are transmitted into the body. The shockwaves stimulate metabolism and the blood circulation, breaking up scar tissues, and resulting in the body’s own healing processes being accelerated. Studies suggest that at least six shockwave treatments are necessary to see the positive results expressed in clinical studies.
Clinical Studies:
Platelets are small biological packages that normally circulate in the blood. They contain many growth factors. The growth factors promote healing by encouraging the growth of news blood vessels to help heal muscles, tendons, ligaments, and cartilage. This healing ability can be harnessed by drawing a small amount of your blood, placing it in a centrifuge to concentrate the platelets, and re-injecting the concentrated platelet-rich plasma (PRP) where your body needs help healing muscles, joints, or tendons. Because joint linings, tendons and ligaments receive very limited blood supply, injecting them with platelet-rich plasma can encourage the growth of new blood vessels and has been shown to accelerate healing and preventing the need for many surgeries.
The body’s ability to repair and replace damaged cartilage, tendon, or other specialized tissue in adults is limited. Injured joints or tendons can be a source of chronic pain and can limit activities. PRP therapy can harness the body’s own healing ability and resources to allow more complete healing than other alternatives. PRP is a natural treatment that uses only your own blood with no other additives.
Clinical Studies:
FOM includes a comprehensive evaluation of the musculoskeletal system to identify range of motion and strength restrictions as well as pain reproducibility. We then direct treatment toward those fascial distortions, the root cause of the symptoms being experienced. With an aim to reduce these fascial distortions while improving motion control and strength. With improved movement, joints and adjacent soft tissues become relieved from the strain which leads to decreased pain as well as increased healing capability in soft tissue.
Clinical Studies:
Platelets are small biological packages that normally circulate in the blood. They contain many growth factors. The growth factors promote healing by encouraging the growth of news blood vessels to help heal muscles, tendons, ligaments, and cartilage. This healing ability can be harnessed by drawing a small amount of your blood, placing it in a centrifuge to concentrate the platelets, and re-injecting the concentrated platelet-rich plasma (PRP) where your body needs help healing muscles, joints, or tendons. Because joint linings, tendons and ligaments receive very limited blood supply, injecting them with platelet-rich plasma can encourage the growth of new blood vessels and has been shown to accelerate healing and preventing the need for many surgeries.
The body’s ability to repair and replace damaged cartilage, tendon, or other specialized tissue in adults is limited. Injured joints or tendons can be a source of chronic pain and can limit activities. PRP therapy can harness the body’s own healing ability and resources to allow more complete healing than other alternatives. PRP is a natural treatment that uses only your own blood with no other additives.
Clinical Studies:
Inflammation can play a role in the development and exacerbation of back pain. When an injury or irritation occurs in the back, the body’s immune response triggers an inflammatory process as a protective mechanism. Inflammation involves the release of various chemicals and immune cells to the affected area, which can lead to pain, swelling, redness, and warmth. The goal of functional medicine testing is to identify and reduce inflammation sources to include food sensitivities, environmental pollutants, and allergies. An inflammatory response to an injury is exacerbated by diet and lifestyle choices causing inflammation that most patients are unaware of.
In the context of back pain, inflammation can affect different structures, including the muscles, ligaments, tendons, and joints in the back. Some ways in which inflammation can contribute to back pain are:
Muscle inflammation: Strained or overworked muscles in the back can become inflamed, causing pain and stiffness. Inflammatory chemicals, such as prostaglandins, can sensitize nerve endings and increase pain perception.
Ligament and tendon inflammation: Inflammation of the ligaments and tendons in the back can result from acute injuries or chronic overuse. Inflammatory processes can cause swelling, pain, and reduced mobility.
Facet joint inflammation: The facet joints are small joints located between the vertebrae in the spine. Inflammation of these joints, often due to arthritis or injury, can lead to localized back pain and stiffness.
Disc inflammation: The discs between the vertebrae can also become inflamed, particularly in cases of herniation or degeneration. Inflammation can contribute to disc-related pain by irritating nearby nerves or sensitizing pain receptors.
In some cases, inflammation in the back can be self-limiting and subside with rest and appropriate care. However, in other instances, chronic inflammation may persist, leading to ongoing or recurrent back pain.
Managing back pain associated with inflammation typically involves a combination of treatments. These may include rest, ice or heat therapy, over-the-counter anti-inflammatory medications (e.g., NSAIDs), physical therapy, exercises to improve flexibility and strength, and, in some cases, corticosteroid injections. It is crucial to consult with a healthcare professional for a proper evaluation and personalized treatment plan for back pain related to inflammation.
Clinical Studies:
Sitting disease is a newer accepted diagnosis in which individuals suffer from back pain due to sitting for extended periods of time. It is advised that individuals stand and take a posture break every hour at a minimum.
It’s important to note that back pain can vary in severity and duration, and multiple factors can contribute to its development. It is advisable to consult with a trusted healthcare professional, like BHS, for an accurate diagnosis and appropriate treatment based on individual circumstances.
While self-treatment for back pain can be helpful for mild cases, it’s important to note that these suggestions are not a substitute for professional medical advice. If you have severe or persistent back pain or any concerning symptoms, it’s recommended to consult with a healthcare professional. Here are some self-care measures that may provide relief for mild back pain:
Preventing back pain involves adopting healthy habits and making lifestyle changes that promote a strong and well-supported back. Here are some tips for preventing back pain:
While these tips can help reduce the risk of back pain, they may not guarantee complete prevention. It’s important to listen to your body, avoid overexertion, and seek professional guidance if you experience persistent or severe back pain.
While many cases of back pain resolve on their own with self-care measures, there are certain situations when it is advisable to see a doctor for evaluation and guidance. Here are some indications to seek medical attention for your back pain:
Remember, these are general guidelines, and individual circumstances may vary. It’s always best to consult with a us for an accurate diagnosis and appropriate treatment based on your specific symptoms and medical history.
The treatment options for back pain depend on the underlying cause, severity of the pain, and individual circumstances. Here are some common treatment approaches:
It’s important to consult with a healthcare professional to determine the most appropriate treatment options based on the underlying cause of your back pain and your individual needs. They can provide a comprehensive evaluation, offer personalized recommendations, and guide you through the treatment process.
Yes, back pain can sometimes be a sign of a more serious underlying condition. While most cases of back pain are due to muscle strains, sprains, or mechanical issues, there are certain conditions that can cause or contribute to back pain and require medical attention.
It’s important to note that experiencing back pain doesn’t automatically mean you have a serious underlying condition. However, if you experience any of the following are associated along with your back pain, it is advisable to seek medical attention promptly:
If you have concerns about your back pain or any associated symptoms, it’s recommended to consult with a BHS provider who can evaluate your condition, perform a thorough examination, and order any necessary tests to determine the underlying cause and provide appropriate treatment.
The duration of back pain can vary widely depending on the underlying cause, severity of the injury or condition, individual factors, and the effectiveness of treatment. In general, acute back pain, which refers to pain that lasts less than 12 weeks, often resolves on its own with conservative measures. However, chronic back pain, lasting 12 weeks or longer, may require more comprehensive management. Here are some general timelines for different types of back pain:
These timelines are general estimates, and the duration of back pain can vary significantly from person to person. Factors such as overall health, individual response to treatment, adherence to self-care measures, inflammation response, and the presence of underlying medical conditions can influence the course and duration of back pain. If your back pain persists or worsens despite conservative measures, it’s advisable to consult with a healthcare professional for a proper evaluation and personalized treatment plan.
There are many exercises and stretches that can help alleviate back pain and promote flexibility, strength, and stability. However, it’s important to note that the specific exercises and stretches that are most beneficial for you may depend on the underlying cause and severity of your back pain. We can help you focus on those exercises and stretches that will be safe and effective for your condition. It’s always a good idea to consult with a healthcare professional, such as a BHS provider, who can assess your condition and provide personalized recommendations. Here are some commonly recommended exercises and stretches for back pain:
Remember to start slowly and gently with these exercises and stretches, and listen to your body. If any exercise or stretch increases your pain or discomfort, stop and consult with a healthcare professional. They can guide you in performing the exercises correctly and provide modifications or additional exercises based on your specific needs.
Breathing is a critical component of any exercise or stretch. As a general rule, it is recommended that you do a minimum of three breaths for each stretch extending the stretch on each exhale and holding the position during your inhales.
Several risk factors can contribute to the development of back pain. Understanding these factors can help you identify potential risks and take preventive measures. Here are some common risk factors for developing back pain:
By adopting a healthy lifestyle, including regular exercise, maintaining proper posture, managing body weight, and practicing safe lifting techniques, you can help reduce your risk of experiencing back pain. If you have specific concerns about your risk factors or back pain, it’s advisable to consult with a BHS professional for further evaluation and guidance.
Making certain lifestyle changes can help reduce back pain and improve your overall spine and musculoskeletal health. Here are some lifestyle modifications that are beneficial:
Stress and emotional factors can contribute to back pain or exacerbate existing back pain. The mind and body are interconnected, and psychological factors can have a significant impact on physical well-being, including the experience of pain. Here’s how stress and emotional factors can influence back pain:
Addressing stress and emotional factors is an important part of managing back pain. Here are some strategies that may help:
While addressing stress and emotional factors can be helpful, it’s also essential to seek appropriate medical care and consult with a healthcare professional for a comprehensive evaluation and management plan for your back pain.
There are ergonomic tips you can follow to maintain good posture and reduce back pain. Here are some recommendations:
It is important to adjust your ergonomic setup based on your individual needs and preferences. If you have specific concerns about your posture or back pain, it’s advisable to consult with a healthcare professional or an ergonomic specialist who can provide personalized recommendations and further guidance.
Certain occupations and activities can increase the likelihood of experiencing back pain. Jobs or activities that involve repetitive movements, heavy lifting, prolonged sitting or standing, or awkward postures can put additional stress on the spine and its supporting structures. Here are some examples:
While these occupations or activities may increase the likelihood of experiencing back pain, it doesn’t mean that everyone in these roles will develop back pain. Proper body mechanics, ergonomic considerations, regular exercise, and taking breaks for stretching and movement can help reduce the risk of back pain in these situations. If you have concerns about back pain related to your occupation or activity, it’s recommended to consult with a healthcare professional or ergonomic specialist for personalized advice and guidance.
Chronic back pain, if left untreated or unmanaged, can lead to several potential complications and long-term effects. Here are some examples:
Chronic back pain can have significant negative effects on quality of life, and appropriate management and treatment can help mitigate these complications. Seeking early medical intervention, developing a comprehensive treatment plan, and adopting lifestyle modifications can improve outcomes and minimize long-term consequences. If you are experiencing chronic back pain, it’s advisable to consult with a healthcare professional who can assess your condition, provide a proper diagnosis, and recommend appropriate treatment options.
The insurance coverage for any treatment, including those for back pain medicine, varies depending on several factors, including the insurance provider, the specific services or treatments being sought, and the healthcare provider’s credentials and billing practices. Here are a few points to consider:
The cost of back pain treatment can vary significantly depending on various factors, including the severity of the condition, the type of treatment required, geographical location, healthcare provider fees, insurance coverage, and any additional diagnostic tests or procedures. At BHS we prioritize the lowest cost and most effective treatment based on your symptoms and condition. Here are some common components that can contribute to the overall cost of back pain treatment:
It’s important to note that the cost of back pain treatment can be significantly influenced by the healthcare system and insurance coverage in your country or region. Having health insurance coverage can help mitigate the out-of-pocket expenses, but specific coverage and reimbursement policies can vary.
To determine the exact cost of back pain treatment, it is recommended to consult with BHS providers, and your primary care physicians, specialists, or insurance representatives, who can provide more specific information based on your individual circumstances. Knowing more information about treatment options and their associated costs will help you make an informed decision about your care.
There can be contraindications or situations where specific treatments for back pain may not be advisable or require caution. It’s important to consult with a BHS provider to assess your individual condition and determine the most appropriate treatment options. Here are some general contraindications for certain back pain treatments:
For Conservative Care therapies:
For Medications:
For Injections or procedures:
For Surgical interventions:
Contraindications can vary depending on the specific treatment modality, individual health status, and other factors. Always consult with a healthcare professional who can evaluate your condition, review your medical history, and provide personalized recommendations regarding any potential contraindications for treating your back pain. They will be able to consider your specific circumstances and advise on the most appropriate and safe treatment options for you.
We focus on addressing the root causes of back and spine pain using advanced regenerative therapies that reduce systemic inflammation, promote healing, and restore mobility. Our approach is non-invasive, avoiding surgeries and addictive medications whenever possible.
We use a combination of cutting-edge therapies tailored to each individual’s needs:
PBM uses light therapy to penetrate deep into tissues, reducing inflammation, easing pain, and speeding up the healing process at a cellular level. It’s effective for both acute injuries and chronic back conditions.
Hydrogen inhalation therapy provides systemic antioxidant effects, neutralizing harmful free radicals and reducing inflammation throughout the body. By lowering oxidative stress, it supports tissue healing and pain relief, especially in chronic conditions.
Extracorporeal Shockwave Therapy (ESWT) delivers acoustic waves to targeted areas, improving blood flow, reducing inflammation, and stimulating tissue repair. It’s highly effective for conditions like herniated discs, sciatica, and chronic back pain.
HIFEM EMS uses electromagnetic energy to contract and strengthen deep muscles that support the spine. By improving muscle stability and spinal alignment, it reduces pain and prevents future injuries.
Systemic inflammation is often a key contributor to chronic pain. By reducing inflammation through therapies like PBM, H2 inhalation, and ESWT, we promote natural healing, reduce reliance on addictive medications, and help many patients avoid invasive surgeries.
Yes! All our therapies are completely non-invasive, safe, and clinically proven to provide effective results without the risks associated with surgeries or long-term use of medications.
Our therapies are suitable for individuals experiencing:
If you’re looking for a non-invasive, drug-free solution, our approach is ideal.
Absolutely! Many of our patients benefit from a customized combination of therapies like PBM, ESWT, H2 inhalation, and hands-on treatments. Our experts will design a personalized plan based on your specific condition and goals.
Results vary depending on the individual and the severity of the condition. Some patients experience noticeable relief after just a few sessions, while others may require several weeks of consistent treatment for optimal results.
Yes! We provide flexible options to fit your lifestyle:
You can start by booking a consultation with our team. We’ll evaluate your condition, discuss your goals, and design a personalized treatment plan to help you achieve long-lasting relief.
See Plans & Pricing
Connect with us over our social platforms & find special deals for you!
© Copyright 2025. All rights reserved.