Discover personalized, non-invasive therapies that address metabolic dysfunction, reduce inflammation, and promote long-term health—delivered in our clinics, at home, or onsite at your workplace.
Diabetes is a chronic condition in which the body cannot effectively regulate blood sugar levels due to insufficient insulin production or resistance to insulin. Prediabetes is a precursor condition where blood sugar levels are elevated but not yet high enough to be classified as diabetes. Both conditions can lead to serious health complications if left untreated, including heart disease, kidney damage, nerve problems, and vision loss. Early intervention and personalized treatments can significantly improve outcomes.


Managing diabetes and prediabetes effectively requires understanding and addressing their root causes. We use advanced genetic testing, nutrigenomics, and pharmacogenetics (PgX) to uncover the unique factors contributing to your condition. Our approach identifies which medications work best for you, addresses hormone imbalances, and provides personalized supplementation to optimize your neuroendocrine system and support the function of vital organs and glands.
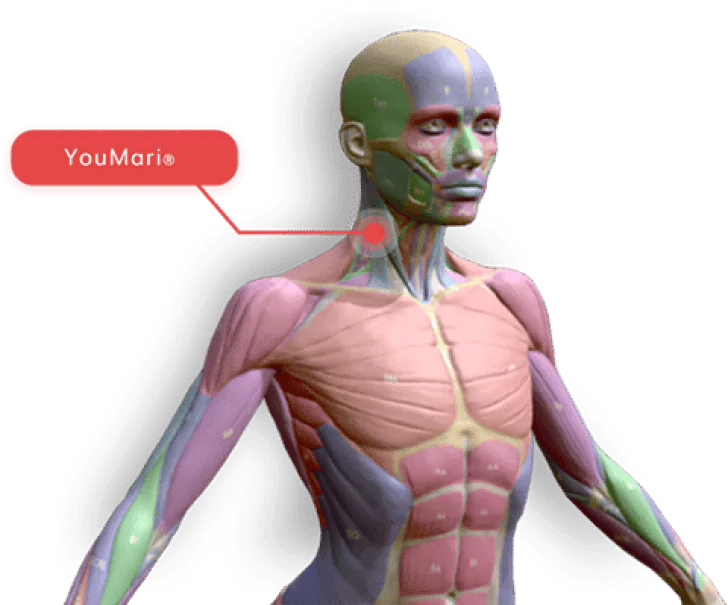
By combining this precision medicine approach with cutting-edge regenerative therapies like photobiomodulation (PBM) and hydrogen inhalation (H2), we target systemic inflammation and promote metabolic healing for sustainable, long-term results.

Experience hands-on care and advanced regenerative therapies in a relaxing, state-of-the-art environment.
Continue your healing journey with easy-to-use devices designed for at-home therapy.
Bring regenerative medicine to your workplace, improving employee health and productivity.
Our Regenerative Therapies our Not the Alternative, they are the
BEST CHOICE
We are committed to personalizing treatment plans based on what is best for every individual’s UNIQUE circumstances to include symptoms, budget, lifestyle, and goals. Conservative (non-pharmaceutical) care is often effective in resolving diabetes and preventing the progression of prediabetes.

We will review your health history, symptoms, and current treatments to help determine the severity of your condition. We may recommend additional testing and analysis to get a full picture of potential therapies personalized to you.
If your condition qualifies for conservative care options, we will present a treatment plan that includes only those therapies proven to be effective in treating your condition. This may include DNA nutrigenomics analysis for lifestyle design, food sensitivities, and other therapies to resolve issues limiting mobility. You will be provided with treatment plan options and timelines with transparent out of pocket costs to you.

Diabetes management can be enhanced through various integrative and regenerative therapies that address underlying mechanisms, improve metabolic health, and support overall well-being.
Nutrigenomics explores how individual genetic variations affect nutrient metabolism and how tailored nutritional interventions can improve health outcomes, including diabetes management.
By analyzing genetic information, nutrigenomics can guide personalized dietary recommendations to optimize blood sugar control and reduce diabetes risk.
Pharmacogenomics examines how genetic variations affect individual responses to medications, allowing for personalized drug therapies in diabetes management.
It helps tailor medication choices to individual genetic profiles, improving efficacy and minimizing adverse effects.
Sleep Studies focus on improving sleep quality, which is crucial for metabolic health and glucose regulation.
Quality sleep supports metabolic function, helps regulate blood sugar levels, and reduces insulin resistance.
Inflammation Programs focus on reducing systemic inflammation through diet, supplements, and lifestyle changes to improve diabetes management.
These programs involve anti-inflammatory diets and supplements to lower chronic inflammation, which is associated with insulin resistance and type 2 diabetes.
Red Light Therapy (or Low-Level Laser Therapy, LLLT) uses specific wavelengths of light to reduce inflammation and improve cellular function.
Red light therapy can enhance cellular metabolism, reduce inflammation, and improve insulin sensitivity, supporting overall diabetes management.
Bioidentical Hormone Therapy uses hormones that are chemically identical to those naturally produced by the body to address hormonal imbalances that can affect diabetes.
Yes, it can help balance hormones involved in glucose metabolism and insulin sensitivity, potentially improving diabetes management.
Bioidentical Hormone Therapy uses hormones that are chemically identical to those naturally produced by the body to address hormonal imbalances that can affect diabetes.
Yes, it can help balance hormones involved in glucose metabolism and insulin sensitivity, potentially improving diabetes management.
For managing diabetes, several integrative and regenerative therapies offer promising benefits:
These therapies can be integrated into a comprehensive approach to diabetes management, addressing various aspects of the condition to improve overall health and well-being.
Increased thirst, frequent urination, fatigue, blurred vision, and unexplained weight loss.
Through lifestyle changes like a healthy diet, regular exercise, weight management, and stress reduction.
Type 1 is an autoimmune condition where the body attacks insulin-producing cells, while Type 2 involves insulin resistance and often relates to lifestyle factors.
While Type 1 diabetes cannot be reversed, Type 2 diabetes and prediabetes can often be managed or improved with lifestyle changes.
Frequency varies by individual and treatment plan, but typically ranges from daily to several times a week.
Potential complications include cardiovascular disease, nerve damage, kidney damage, and vision problems.
Medications may be necessary to control blood sugar levels, but lifestyle changes remain crucial for effective management.
Genetics play a significant role in diabetes, influencing susceptibility to both Type 1 and Type 2 diabetes.
Nutrigenomics is the study of how genetic variations affect individual responses to nutrients and how this information can be used to tailor dietary recommendations for better health outcomes.
Nutrigenomics can provide personalized dietary advice that helps optimize blood sugar control, reduce the risk of diabetes, and improve overall metabolic health.
Pharmacogenomics examines how genetic differences influence individual responses to medications, allowing for more personalized and effective drug therapies.
By identifying genetic markers that affect drug metabolism, pharmacogenomics can help tailor medication choices to individual patients, improving efficacy and reducing side effects.
Sleep Studies focus on improving sleep quality and duration, which are crucial for maintaining healthy metabolic function and glucose regulation.
Quality sleep supports metabolic health, improves insulin sensitivity, and can reduce the risk of developing type 2 diabetes.
Inflammation Programs aim to reduce systemic inflammation through dietary changes, supplements, and lifestyle modifications, which can positively impact insulin sensitivity and glucose metabolism.
By addressing chronic inflammation, these programs can improve insulin sensitivity and reduce diabetes risk.
Red Light Therapy (or Low-Level Laser Therapy, LLLT) uses specific wavelengths of light to enhance cellular function, reduce inflammation, and improve metabolic health.
Red light therapy can improve insulin sensitivity, reduce oxidative stress, and support overall metabolic health.
Bioidentical Hormone Therapy involves using hormones that are chemically identical to those naturally produced by the body to address hormonal imbalances that can affect blood sugar levels and insulin sensitivity.
By restoring hormonal balance, bioidentical hormone therapy can help regulate glucose metabolism and improve insulin sensitivity.
Shockwave Therapy (Extracorporeal Shock Wave Therapy) uses acoustic waves to improve circulation, reduce inflammation, and support metabolic function.
ESWT may enhance blood flow and reduce inflammation, which could support metabolic health and improve diabetes management.
These approaches can be integrated into a comprehensive diabetes management plan to address various aspects of the condition and improve overall health outcomes.
Diabetes is a chronic condition where the body struggles to regulate blood sugar levels due to insulin resistance or insufficient insulin production. Prediabetes is a precursor to diabetes, characterized by elevated blood sugar levels that are not yet high enough to be classified as diabetes.
PBM enhances mitochondrial function, improving cellular energy production (ATP) and reducing inflammation. This supports insulin sensitivity and overall metabolic health.
Hydrogen inhalation therapy provides systemic antioxidant effects, reducing oxidative stress and inflammation—two major contributors to insulin resistance and metabolic dysfunction.
DNA genetic testing and nutrigenomics uncover genetic predispositions that affect how your body processes nutrients, enabling the creation of a personalized dietary strategy to improve metabolic health and glucose regulation.
Pharmacogenetics analyzes your genetic profile to determine which medications will be most effective and safe for your body, ensuring optimal outcomes for managing diabetes and prediabetes.
Yes, hormone imbalances can significantly affect glucose regulation and metabolic health. Our approach includes identifying and correcting imbalances to optimize the neuroendocrine system and improve organ function.
Personalized supplementation provides targeted nutrients to support vital organ function, improve insulin sensitivity, and promote metabolic healing.
Yes! All our therapies are non-invasive, safe, and designed for consistent use without harmful side effects, making them ideal for long-term diabetes and prediabetes management.
In many cases, our therapies improve metabolic function and blood sugar control, potentially reducing the need for medications or preventing progression to conditions that require more intensive treatment.
Our therapies are ideal for individuals who:
Results vary depending on the individual, but many patients experience improvements in energy levels, inflammation, and blood sugar regulation within a few weeks of starting treatment.
Absolutely. Our therapies complement traditional treatments like lifestyle changes and medications, enhancing their effectiveness for better outcomes.
Book a consultation with our team to assess your condition, discuss your goals, and develop a personalized plan to support your metabolic health and prevent complications.
See Plans & Pricing
Connect with us over our social platforms & find special deals for you!
© Copyright 2025. All rights reserved.