Discover advanced therapies, tailored to your needs, that can be delivered in our clinics, at home, or onsite at your workplace.
Plantar fasciitis is a common condition that causes pain in the heel and bottom of the foot. It occurs when the plantar fascia—a thick band of tissue that connects the heel bone to the toes—becomes inflamed or strained. Often linked to overuse or improper support, plantar fasciitis can be debilitating and affect daily activities such as walking, standing, or exercising. This condition is one of the leading causes of heel pain and affects millions of individuals annually.


Plantar fasciitis can have various causes, including:
Plantar fasciitis can cause debilitating heel and foot pain, making it difficult to walk, stand, or perform daily activities. We combine advanced regenerative therapies to address the root causes of pain, reduce inflammation, and promote natural tissue repair—helping you avoid surgery or long-term reliance on medications.
Our tailored treatment plans provide targeted relief, strengthening the surrounding muscles and restoring foot function for lasting results.

Experience hands-on care and advanced regenerative therapies in a relaxing, state-of-the-art environment.
Continue your healing journey with easy-to-use devices designed for at-home therapy.
Bring regenerative medicine to your workplace, improving employee health and productivity.
Our Regenerative Therapies our Not the Alternative, they are the
BEST CHOICE
We are committed to personalizing treatment plans based on what is best for every individual’s UNIQUE circumstances to include symptoms, budget, lifestyle, and goals. Conservative (non-surgical) care is effective in resolving pain and injuries most of the time.

We will evaluate your health history, symptoms, and conduct functional movement tests to help determine the severity of your condition. In some cases, additional evaluation may be needed. This can involve X-rays to assess bone structure, MRI scans to visualize soft tissues, or ultrasound for specific conditions. These imaging methods help us achieve a more accurate diagnosis.
If your condition qualifies for conservative care options, we will present a treatment plan that includes only those modalities proven to be effective in treating your condition. This may include shockwave, PRP, light therapy, and fascial manipulation. You will be provided with at least treatment plan options and timelines with transparent out of pocket costs to you.

In general, studies suggest that approximately 60% to 80% of individuals with knee pain experience significant improvement and pain relief through conservative measures. These conservative treatments may include physical therapy, exercise, medication management, lifestyle modifications, and orthotic devices. Conservative care treatments work best when spread out over a 3 to 6-week period to allow adequate healing between treatment modalities.
If your symptoms and condition is not eligible for conservative care, or conservative care did not produce the desired outcomes, we start with an expert/accurate diagnosis from our medical doctor pain specialists. Our medical director (6-time patented medical device inventor) will personally conduct a 90-minute comprehensive evaluation to include reviewing available imaging resulting in an accurate diagnosis and personalized treatment plan options.


our goal is to resolve pain, improve strength, and improve range of motion without surgery. We are consistently successful in achieving this in over 90% of cases. In those rare cases in which surgery is necessary we will guide you by finding the right surgeon we trust for your particular injury and circumstances. We are your independent experts and not financially motivated to conduct surgeries.
Extracorporeal Shockwave Therapy (ESWT), also known as Pulsewave, is a breakthrough technology for stimulating healing of chronic pain and musculoskeletal injuries. ESWT is also referred to as PulseWave therapy. In simple terms, both use high-energy sound waves outside of the body to improve blood flow and initiate the bodies’ own healing processes. This is effective in both chronic and acute injuries. There has been significant, successful, research on the efficacy of ESWT for injuries.
Shockwaves can accelerate the healing process in the body, they stimulate metabolism and improve blood circulation; allowing damaged tissue to regenerate and fully heal. When properly applied, shockwave therapy can take a chronic condition knee into the acute phase of healing. Chronic pain is caused by an incomplete healing process which must be disrupted (signaled) to be resolved (fully healed). ESWT has been used and studied in clinical applications since 1980, first emerging as a noninvasive procedure to breakup kidney stones. Treatment is noninvasive and virtually painless. The provider moves a handpiece around the pain zone and through the wand, low-energy shockwaves are transmitted into the body. The shockwaves stimulate metabolism and the blood circulation, breaking up scar tissues, and resulting in the body’s own healing processes being accelerated. Studies suggest that at least six shockwave treatments are necessary to see the positive results expressed in clinical studies.
Clinical Studies:
Platelets are small biological packages that normally circulate in the blood. They contain many growth factors. The growth factors promote healing by encouraging the growth of news blood vessels to help heal muscles, tendons, ligaments, and cartilage. This healing ability can be harnessed by drawing a small amount of your blood, placing it in a centrifuge to concentrate the platelets, and re-injecting the concentrated platelet-rich plasma (PRP) where your body needs help healing muscles, joints, or tendons. Because joint linings, tendons and ligaments receive very limited blood supply, injecting them with platelet-rich plasma can encourage the growth of new blood vessels and has been shown to accelerate healing and preventing the need for many surgeries.
The body’s ability to repair and replace damaged cartilage, tendon, or other specialized tissue in adults is limited. Injured joints or tendons can be a source of chronic pain and can limit activities. PRP therapy can harness the body’s own healing ability and resources to allow more complete healing than other alternatives. PRP is a natural treatment that uses only your own blood with no other additives.
Clinical Studies:
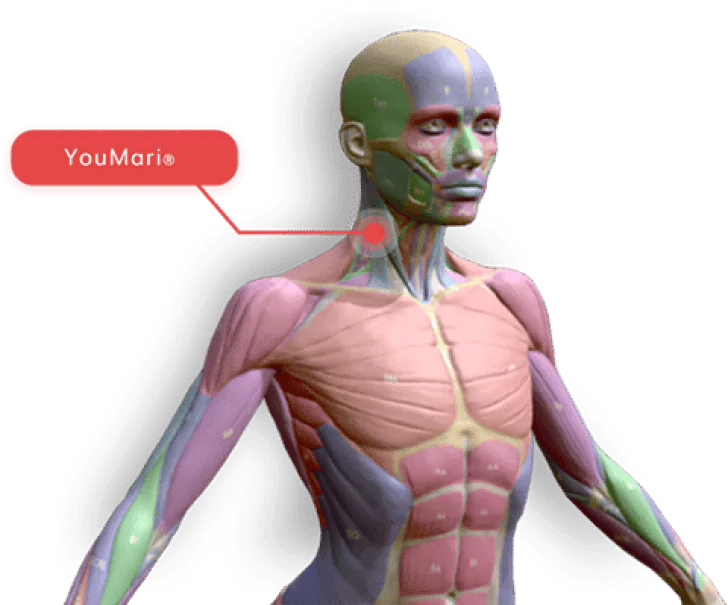
Fascial manipulation represents a wide array of scientifically-validated treatment techniques and models utilizing manual therapy that targets muscles and fascia in order to resolve pain, musculoskeletal injuries, and improve range of motion and strength. We utilize Functionally Optimized Massage ™ (FOM) which has effectively combined these techniques and models proven effective for specific injuries; however, no one technique has been proven effective on all 150 plus musculoskeletal conditions except our FOM.
FOM includes a comprehensive evaluation of the musculoskeletal system to identify range of motion and strength restrictions as well as pain reproducibility. We then direct treatment toward those fascial distortions, the root cause of the symptoms being experienced. With an aim to reduce these fascial distortions while improving motion control and strength. With improved movement, joints and adjacent soft tissues become relieved from the strain which leads to decreased pain as well as increased healing capability in soft tissue.
Clinical Studies:
Platelets are small biological packages that normally circulate in the blood. They contain many growth factors. The growth factors promote healing by encouraging the growth of news blood vessels to help heal muscles, tendons, ligaments, and cartilage. This healing ability can be harnessed by drawing a small amount of your blood, placing it in a centrifuge to concentrate the platelets, and re-injecting the concentrated platelet-rich plasma (PRP) where your body needs help healing muscles, joints, or tendons. Because joint linings, tendons and ligaments receive very limited blood supply, injecting them with platelet-rich plasma can encourage the growth of new blood vessels and has been shown to accelerate healing and preventing the need for many surgeries.
The body’s ability to repair and replace damaged cartilage, tendon, or other specialized tissue in adults is limited. Injured joints or tendons can be a source of chronic pain and can limit activities. PRP therapy can harness the body’s own healing ability and resources to allow more complete healing than other alternatives. PRP is a natural treatment that uses only your own blood with no other additives.
Clinical Studies:
“Based on the evidence synthesis there is Level III evidence for intradiscal injections of PRP and MSCs, whereas the evidence is considered Level IV for lumbar facet joint, lumbar epidural, and sacroiliac joint injections of PRP, (on a scale of Level I through V) using a qualitative modified approach to the grading of evidence based on best evidence synthesis.”https://pubmed.ncbi.nlm.nih.gov/30717500/
Inflammation can play a role in the development and exacerbation of knee pain. When an injury or irritation occurs in the knee, the body’s immune response triggers an inflammatory process as a protective mechanism. Inflammation involves the release of various chemicals and immune cells to the affected area, which can lead to pain, swelling, redness, and warmth. The goal of functional medicine testing is to identify and reduce inflammation sources to include food sensitivities, environmental pollutants, and allergies. An inflammatory response to an injury is exacerbated by diet and lifestyle choices causing inflammation that most patients are unaware of.
In the context of knee pain, inflammation can affect different structures, including the muscles, ligaments, tendons, and joints in the knee. Some ways in which inflammation can contribute to knee pain are:
Muscle inflammation: Strained or overworked muscles in the knee can become inflamed, causing pain and stiffness. Inflammatory chemicals, such as prostaglandins, can sensitize nerve endings and increase pain perception.
Ligament and tendon inflammation: Inflammation of the ligaments and tendons in the knee can result from acute injuries or chronic overuse. Inflammatory processes can cause swelling, pain, and reduced mobility.
In some cases, inflammation in the knee can be self-limiting and subside with rest and appropriate care. However, in other instances, chronic inflammation may persist, leading to ongoing or recurrent knee pain.
Managing knee pain associated with inflammation typically involves a combination of treatments. These may include rest, ice or heat therapy, over-the-counter anti-inflammatory medications (e.g., NSAIDs), physical therapy, exercises to improve flexibility and strength, and, in some cases, corticosteroid injections. It is crucial to consult with a healthcare professional for a proper evaluation and personalized treatment plan for knee pain related to inflammation.
Clinical Studies:
Plantar fasciitis can have a variety of underlying causes. The most common causes of plantar fasciitis include:
These are common causes of knee pain, but the specific underlying issue may vary from person to person. Consultation with a healthcare professional is essential to determine the exact cause and develop an appropriate treatment plan.
Self-treatment for knee pain can be a helpful part of managing discomfort and promoting recovery. However, it’s important to remember that these measures should complement, not replace, professional medical advice. Here are some self-care strategies for knee pain:
Remember, if your knee pain persists, worsens, or significantly impairs your mobility, it’s crucial to consult a healthcare professional for a proper diagnosis and personalized treatment plan. They can provide expert guidance and recommend specific interventions tailored to your condition.
Preventing knee pain involves adopting lifestyle changes and habits that support knee joint health. Here are some strategies to help prevent knee pain:
Remember that prevention is key, and maintaining overall joint health can go a long way in preventing knee pain. If you do experience persistent or severe knee pain, consult with a healthcare professional for a proper diagnosis and treatment plan.
While many cases of knee pain resolve on their own with self-care measures, there are certain situations when it is advisable to see a doctor for evaluation and guidance. Here are If you’re experiencing knee pain, it’s important to know when to seek medical attention. While some minor knee discomfort may resolve on its own with rest and self-care, there are situations where consulting a doctor is advisable. Here are some guidelines for when to see a doctor for knee pain:
In general, if you’re unsure whether your knee pain requires medical attention, it’s better to err on the side of caution and consult a BHS healthcare professional. They can perform a thorough evaluation, recommend appropriate tests or imaging, and provide guidance on treatment options to help you manage your knee pain effectively. Early diagnosis and treatment often lead to better outcomes and a faster recovery.
The treatment options for knee pain depend on the underlying cause, severity of the pain, and individual circumstances. Here are some common treatment approaches:
The choice of treatment should always be tailored to your specific condition, as well as your personal preferences and goals. BHS healthcare professionals will perform a thorough evaluation, including diagnostic tests, to determine the most appropriate treatment plan for your knee pain. Your active involvement and communication with your healthcare team at BHS are essential for achieving the best outcomes in managing knee pain.
Certainly, here are the potential red flags indicating that knee pain may be a sign of a more serious underlying condition:
It’s essential to note that knee pain is common and often associated with non-serious conditions like overuse or minor injuries. However, if you have concerns about your knee pain, especially if it’s associated with any of the red flags mentioned above, consult a healthcare provider for a comprehensive evaluation, diagnosis, and appropriate management. Early detection and treatment of underlying conditions can significantly impact outcomes and overall health.
The duration of knee pain can vary widely based on the underlying cause and the effectiveness of treatment. Research indicates that the length of knee pain can be influenced by several factors:
It’s important to note that while knee pain may have an expected duration based on the underlying cause, individual experiences can vary. Prompt and appropriate treatment is crucial to managing knee pain effectively and improving one’s quality of life. If you are experiencing knee pain, it’s advisable to consult with a healthcare professional for a thorough evaluation and personalized treatment plan.
Exercises and stretches can be beneficial for alleviating knee pain, but the specific exercises should be tailored to the underlying cause of your knee pain. It’s essential to consult with a healthcare professional or a physical therapist for a personalized exercise plan. Here are some common exercises and stretches that may help relieve knee pain:
Remember to start with low-impact exercises and stretches, and progress gradually. If you experience increased pain or discomfort during any exercise, stop and consult a healthcare professional. The effectiveness of exercises and stretches may vary depending on the underlying cause of your knee pain, so consult with a healthcare provider for a proper diagnosis and guidance on the most suitable exercises for your condition.
Several risk factors can contribute to the development of knee pain. Understanding these factors can help you identify potential risks and take preventive measures. Here are some common risk factors for developing knee pain:
It’s essential to understand that the presence of these risk factors does not guarantee the development of knee pain. Some risk factors are modifiable, meaning that lifestyle changes, physical therapy, and preventive measures can help reduce the risk. Maintaining a healthy weight, staying physically active, and using proper techniques in sports or work activities can decrease the likelihood of knee pain. If you have concerns about your knee health or experience persistent knee pain, it’s advisable to consult a healthcare provider for an accurate diagnosis and guidance on appropriate preventive measures.
Making certain lifestyle changes can help reduce knee pain and improve your overall spine and musculoskeletal health. Here are some lifestyle modifications that are beneficial:
Consult with a healthcare provider or physical therapist to establish a personalized plan addressing your specific knee pain. They can provide tailored guidance, exercises, and treatments to meet your individual needs. A combination of lifestyle adjustments and appropriate medical care can significantly alleviate knee pain and enhance overall joint health.
stress and emotional factors can contribute to knee pain. The connection between emotional well-being and physical pain is well-documented, and knee pain is no exception. Here’s how stress and emotions can impact knee pain:
To address knee pain related to stress and emotions, it’s important to adopt a holistic approach that considers both physical and emotional well-being:
It’s crucial to consult with a healthcare provider to evaluate the specific causes of knee pain and discuss a comprehensive approach that addresses both physical and emotional well-being. This approach may include tailored treatments, therapies, or lifestyle changes to manage and alleviate knee pain related to stress and emotions.
There are ergonomic tips you can follow to maintain good posture and reduce knee pain.
Sit with proper posture:
Use a chair that provides good lumbar support or consider using a lumbar cushion. Sit with your knee against the chair and your feet flat on the floor. Keep your knees at a 90-degree angle and your thighs parallel to the floor. Maintain a small gap between the knee of your knees and the edge of the seat. Avoid crossing your legs, as it can contribute to poor posture.
Set up your workstation ergonomically:
Adjust the height of your chair so that your elbows are at a 90-degree angle and your forearms are parallel to the floor. Position your computer monitor at eye level, directly in front of you, to avoid straining your neck. Use a document holder if you frequently refer to documents while working on the computer. Place frequently used items within easy reach to minimize unnecessary twisting or reaching.
Use an ergonomic keyboard and mouse:
Use a keyboard that allows your wrists to remain in a neutral position, avoiding excessive bending or extension. Consider using a mouse pad with a wrist rest to support your wrist during mouse usage. Take regular breaks and perform stretching exercises for your hands, wrists, and fingers.
Stand with proper posture:
If you have a standing desk, ensure that it is adjusted to the appropriate height so that your wrists are in a neutral position when typing. Stand with your weight evenly distributed on both feet and avoid leaning forward or backward. Use a footrest if necessary to provide support and reduce fatigue.
Lift objects correctly:
Bend your knees and hips while keeping your knee straight when lifting objects from the ground. Hold objects close to your body and avoid twisting or jerking motions. If the object is too heavy, ask for assistance or use lifting aids or equipment.
Take regular breaks and move:
Avoid prolonged periods of sitting or standing. Take short breaks every 30 minutes to stand up, stretch, and move around. Perform gentle stretching exercises for your knee, neck, and shoulders to relieve tension and improve circulation.
Use supportive footwear:
Wear comfortable shoes with good arch support and cushioning to maintain proper alignment and reduce strain on your knee.
Maintain a neutral sleeping position:
Use a mattress and pillow that provide adequate support for your spine. Avoid excessively firm or sagging mattresses. Choose a pillow that keeps your neck in alignment with your spine and supports the natural curvature of your neck. It is important to adjust your ergonomic setup based on your individual needs and preferences. If you have specific concerns about your posture or knee pain, it’s advisable to consult with a healthcare professional or an ergonomic specialist who can provide personalized recommendations and further guidance.
Certain occupations and activities can increase the likelihood of experiencing knee pain. Knee pain can result from repetitive movements, excessive strain, or prolonged periods of stress on the knee joint. Here are some examples of occupations and activities that may contribute to knee pain:
To reduce the risk of knee pain in these occupations and activities, individuals should consider the following:
Occupational or activity-related knee pain can often be managed with proper precautions, exercise, and ergonomics. However, if knee pain becomes chronic or severe, it’s essential to seek medical evaluation and treatment to prevent further complications.
Chronic knee pain can result in several potential complications and long-term effects if not properly managed or treated. These complications can significantly impact an individual’s daily life and overall well-being. Here are some potential complications and long-term effects of chronic knee pain:
To prevent these complications and long-term effects, individuals experiencing chronic knee pain should seek medical evaluation and develop a comprehensive treatment plan. This plan may include physical therapy, medication, lifestyle modifications, and, in some cases, surgical interventions. Early intervention and appropriate management can help improve mobility, reduce pain, and enhance an individual’s overall well-being.
The insurance coverage for any treatment, including those for knee pain medicine, varies depending on several factors, including the insurance provider, the specific services or treatments being sought, and the healthcare provider’s credentials and billing practices. Here are a few points to consider:
To determine the insurance coverage for services, it is advisable to contact your insurance provider directly and inquire about the specific services or treatments you are considering. Additionally, you can reach out to BHS practitioners you are considering working with to discuss billing practices, insurance coverage, and potential reimbursement options.
Remember that insurance coverage can be complex and can vary widely, so it’s important to gather accurate and up-to-date information from both your insurance provider and the practitioner to make informed decisions about your healthcare and associated costs.
The cost of knee pain treatment can vary significantly depending on various factors, including the severity of the condition, the type of treatment required, geographical location, healthcare provider fees, insurance coverage, and any additional diagnostic tests or procedures. At BHS we prioritize the lowest cost and most effective treatment based on your symptoms and condition. Here are some common components that can contribute to the overall cost of knee pain treatment:
It’s important to note that the cost of knee pain treatment can be significantly influenced by the healthcare system and insurance coverage in your country or region. Having health insurance coverage can help mitigate the out-of-pocket expenses, but specific coverage and reimbursement policies can vary.
To determine the exact cost of knee pain treatment, it is recommended to consult with BHS providers, and your primary care physicians, specialists, or insurance representatives, who can provide more specific information based on your individual circumstances. Knowing more information about treatment options and their associated costs will help you make an informed decision about your care.
There can be contraindications or situations where specific treatments for knee pain may not be advisable or require caution. It’s important to consult with a BHS provider to assess your individual condition and determine the most appropriate treatment options. Here are some general contraindications for certain knee pain treatments:
For Conservative Care therapies:
For Medications:
For Injections or procedures:
For Surgical interventions:
Contraindications can vary depending on the specific treatment modality, individual health status, and other factors. Always consult with a healthcare professional who can evaluate your condition, review your medical history, and provide personalized recommendations regarding any potential contraindications for treating your knee pain. They will be able to consider your specific circumstances and advise on the most appropriate and safe treatment options for you.
Plantar fasciitis is the inflammation of the plantar fascia, the thick band of tissue connecting the heel to the toes. This condition is a leading cause of heel pain and often results from overuse, poor footwear, or foot structure abnormalities.
PBM uses specific wavelengths of light to reduce inflammation, increase blood flow, and accelerate cellular repair in the plantar fascia, promoting faster healing and long-term relief.
Extracorporeal Shockwave Therapy (ESWT) delivers acoustic waves to the damaged tissue, stimulating healing, improving circulation, and breaking down scar tissue in the plantar fascia.
Yes! Our non-invasive therapies are highly effective in reducing pain and promoting healing, helping most patients avoid the need for surgery or long-term reliance on medications.
H2 inhalation therapy reduces systemic inflammation and oxidative stress, creating a supportive environment for faster tissue healing and pain relief.
HIFEM EMS strengthens the muscles in the foot and lower leg, reducing strain on the plantar fascia and improving overall stability, which helps prevent future injuries.
Yes! Hands-on fascial massage releases tension, improves flexibility in the foot, and addresses underlying imbalances in the surrounding muscles and tissues that contribute to pain.
Results vary based on the severity of the condition, but many patients experience significant pain relief within a few sessions. Consistent treatment enhances long-term outcomes.
Absolutely. All our therapies are non-invasive, safe, and clinically proven, making them ideal for patients seeking effective pain relief without risks.
Yes, our PBM and H2 devices are easy to use at home, allowing you to continue your recovery conveniently between clinic visits.
Our therapies are suitable for individuals with:
Book a consultation with our team today. We’ll assess your condition, discuss your goals, and create a personalized treatment plan to help you heal and get back on your feet.
See Plans & Pricing
Connect with us over our social platforms & find special deals for you!
© Copyright 2025. All rights reserved.